Publications
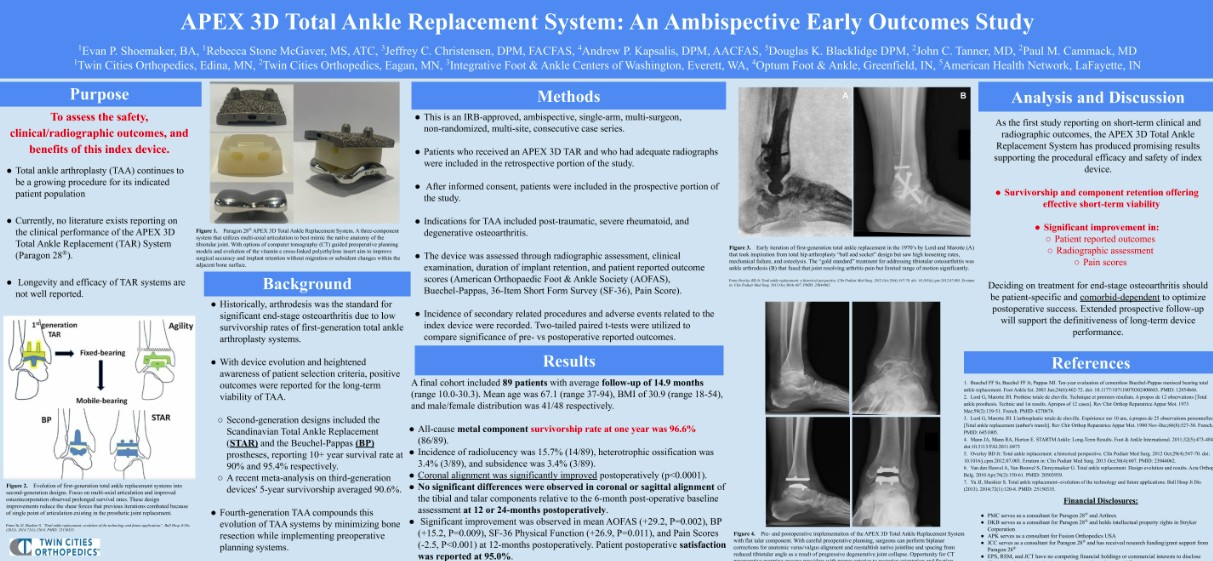
APEX 3D™ Total Ankle Replacement System: An Ambispective Early Outcomes Study
Shoemaker EP, McGaver RS, Christensen JC, Kapsalis AP, Blacklidge DK, Tanner JC, Cammack PM
American College of Foot and Ankle Surgeons Scientific Conference, March 2025; Phoenix, AZ
Eight-nine patients who underwent total ankle replacements with the APEX 3D® Total Ankle Replacement System were retrospectively reviewed. All-cause metal component survivorship at one-year post-operative was 96.6%. Coronal and sagittal radiographic views showed statistically significant improvement and maintenance of alignment respectively of both the tibial and talar components. Incidence of radiolucency was 15.7%, heterotrophic ossification was 3.4%, and subsidence was 3.4%. In patients who agreed to provide prospective patient reported outcome measures, significant improvement was observed 12-months post-operatively in mean AOFAS, SF-36 Physical Function, and pain scores, and patient satisfaction was reported at 95.0%.
Syndesmotic Fixation Utilizing a Novel Screw A Retrospective Case Series Reporting Early Clinical and Radiographic Outcomes
Stenquist D, Velasco BT, Cronin PK, Briceño J, Miller CP, Riedel MD, Kwon JY
Foot & Ankle Specialist. 2020; 13(5), 397-403.
A retrospective review of 18 consecutive patients (with 24 screws) who underwent syndesmotic fixation utilizing a Paragon 28® R3LEASE™ screw was conducted. Mean follow-up was 11.7 months (range: 6.0-14.7 months). 5 of 24 R3LEASE™ screws were broken at an average of 154.8 days (range: 80-196 days) after implantation. All 5 R3LEASE™ screws broke at the intended break point. There was no syndesmotic diastasis, mortise malalignment, or surgical complications. No R3LEASE™ screws were removed.
Related Product: R3LEASE™ Stabilization System
Proximal Rotational Metatarsal Osteotomy for Hallux Valgus (PROMO): Short-term Prospective Case Series With a Novel Technique and Topic Review
Wagner P, Wagner E
Foot & Ankle Orthopaedics. 2018; 3(3)
Twenty-five patients (30 feet) who underwent hallux valgus correction with the Proximal Rotational Metatarsal Osteotomy (PROMO) technique were prospective followed for an average of 12 months. Patients were allowed to bear weight immediately, as tolerated. 100% of the patients were satisfied with the procedure. Radiographic and functional improvements were found. One patient did not have complete rotational correction. There were no infections, deep venous thrombosis, or radiologic recurrence at final follow-up.
Related Product: PROMO™ Triplanar Hallux Valgus Correction System
Is the Rotational Deformity Important in Our Decision-Making Process for Correction of Hallux Valgus Deformity?
Wagner P, Wagner E
Foot and Ankle Clinics. 2018; 23(2), 205-217.
The authors provide commentary on how the rotational deformity influences their procedure choice for hallux valgus correction and discuss when they use a Proximal Metatarsal Rotational Osteotomy (PROMO) technique. Results on 25 patients with average follow-up of 1 year showed improved lower extremity function with no recurrences, complications, secondary metatarsalgia, dorsal malunion, or metatarsal shortening.
Related Product: PROMO™ Triplanar Hallux Valgus Correction System
Proximal Rotational Metatarsal Osteotomy for Treatment of Hallux Valgus: A Technique Guide
Wallace SB, Hunt KJ
Techniques in Foot & Ankle Surgery. 2021
The authors provide a technique guide for their preferred Proximal Rotational Metatarsal Osteotomy system, the Paragon 28® PROMO Triplanar Hallux Valgus Correction System. The authors note that patients are made non-weight-bearing in a splint for 1 to 2 weeks, followed by a walking boot for 6 weeks. A sample case is provided with no deformity recurrence at 1 year.
Related Product: PROMO™ Triplanar Hallux Valgus Correction System
The Use of a Triplanar Metatarsal Rotational Osteotomy to Correct Hallux Valgus Deformities
Wagner P, Wagner E
JBJS essential surgical techniques. 2019; (9)4
The authors provide a technique guide for the Proximal Rotational Metatarsal Osteotomy system using the Paragon 28® PROMO Triplanar Hallux Valgus Correction System. A narrated surgical video is provided with commentary on the procedure, results, and post-operative protocol.
Related Product: PROMO™ Triplanar Hallux Valgus Correction System
Role of Coronal Plane Malalignment in Hallux Valgus Correction
Wagner P, Wagner E
Foot and ankle clinics. 2020; (25)1, 69-77
The authors discuss the coronal plane deformity associated with hallux valgus and some of the surgical options used to treat the deformity. Clinical outcomes on the Proximal Rotational Metatarsal Osteotomy are reported on 60 patients with 1 year of follow-up and 25 patients with 2 years of follow-up. Two cases of deformity relapse were seen. There was 1 delayed union that progressed to union at 3 months. No infections were seen.
Related Product: PROMO™ Triplanar Hallux Valgus Correction System
Flexor tenodesis procedure in the treatment of lesser toe deformities
de Cesar Netto C, Schmidt EL, Lalevee M, Mansur NSB
Archives of Orthopaedic and Trauma Surgery. 2021; 1-13
A flexor tenodesis procedure is described using the Paragon 28® TenoTac™ Soft Tissue Fixation System. Three lesser toe deformity case summaries are presented with average follow-up of 6.3 months. All patients showed improved patient reported outcome scores. The authors report good clinical and radiographic correction with no complications related to the implant or technique.
Related Product: TenoTac® Soft Tissue Fixation System
Biomechanical Comparison of First Tarsometatarsal Arthrodesis Constructs Over Prolonged Cyclic Testing
Prieto-Diaz C, Anderle MR, Brinker LZ, Allard R, Leasure J
Foot & Ankle Orthopaedics. 2019; 4(4)
A biomechanical experiment was conducted on forty cadaver specimens that received 1 of 4 operative treatments: a Phantom® Intramedullary Nail with 2 points of fixation in the cuneiform, a Phantom® Intramedullary Nail with 1 point of fixation in the cuneiform, a Gorilla® Lapidus plate, or 2 crossing screws. Both versions of the Phantom® Intramedullary Nail, and the Gorilla® Lapidus plate resisted plantar gapping better that two crossing screws.
Related Products:
Percutaneous Modified Lapidus Procedure with Early Weightbearing: Technique and Early Outcomes of the First 30 Cases
Bean B, Mangold DR, Abousayed M, Coleman MM, Thompson J, Guyton G
Foot & Ankle Orthopaedics. 2022; 7(1)
A retrospective review was conducted on the first 30 consecutive percutaneous MIS-modified Lapidus procedures by a single surgeon utilizing the Phantom® Intramedullary Nail. Pain scores, IMA, and HVA all improved from pre-operative to post-operative. There were no intraoperative complications, or post-operative wound complications, surgical site infections, hardware complications, transfer metatarsalgia, or nerve-related problems. There was 1 case of hallux valgus recurrence and 1 nonunion which required revision.
Related Product: Phantom® Intramedullary Nail
A bi-radial approach to define the sagittal geometry of the healthy ankle
Anderle MR, Obert RM, Paxson RD, Brinker LZ, Clancy JT
Foot and Ankle Surgery. 2021; 27(7)
Weightbearing CT scans were used to analyze the sagittal curvature of the talar dome and distal tibia in 18 healthy subjects. The curvature at four anatomic regions (Lateral Posterior, Medial Posterior, Lateral Anterior, and Medial Anterior) was found. For the talus, the medial anterior radius was smaller than the lateral anterior radius. For the distal tibia, the lateral posterior radius was smaller than the medial posterior radius. The most common geometric configuration was two cones, one anterior and one posterior, pointed in opposite directions.
Related Product:
APEX 3D™ Total Ankle Replacement System
Early results and complication rate of the LapiCotton procedure in the treatment of medial longitudinal arch collapse: a prospective cohort study
de Cesar Netto C, Ehret A, Walt J, Chinelati RM, Dibbern K, de Carvalho KA, Tazegul TE, Lalevee M, Mansur NS
Archives of Orthopaedic and Trauma Surgery. 2022 Mar 21:1-3.
Outcomes from 22 patients who underwent a LapiCotton procedure with a PRESERVE™ Lapidus Angular Length Restoring Graft were reported. Intra-operatively, trial sizers were used to determine the appropriate size of the graft. The median size of the PRESERVE™ graft used was 8 mm (range: 5-19 mm). A variety of fixation methods were employed. At 3-months post-op, 91% of the subjects (20/22 subjects) achieved complete healing of both surfaces of the fusion site. Statistically significant improvement was seen in the talus-first metatarsal angle from pre-operatively to post-operatively (p<.0001). One patient required reoperation.
Related Product: PRESERVE™ Bone and Biologic Solutions
Orthogonal Locked Plating for Tibiotalocalcaneal Arthrodesis
Ciufo DJ, Grant AM
Techniques in Foot & Ankle Surgery, 21(1), 40-47.
The authors share a technique for TTC arthrodesis using the anatomically contoured Silverback™ TT/TTC Plating System. Four cases are summarized with two of the cases presented in detail. All patients went on to fusion and were satisfied with the procedure. All patients reported pain scores of 0 or 1 (out of 10) at the most recent follow-up. No reoperations were required. One subject had plantar nerve pain after the procedure which gradually decreased over time.
Related Product:
Silverback™ TT/TTC Plating System
A Large Animal Model for Orthopedic Foot and Ankle Research
Gadomski BC, Labus KM, Stewart HL, Bisazza KT, Nelson BB, Puttlitz CM, McGilvray KC, Regan DP, Easley JT
Frontiers in Veterinary Science. 2022;9.
A novel large animal model was developed for the investigation of foot and ankle implants. 8 sheep underwent ligament resection and subsequent stabilization with canulated Mini-Monster® Screws. 2 additional sheep served as controls. 4 of the surgically stabilized animals were sacrificed at 6 weeks and the remaining four at 10 weeks. Arthritic changes were noted in 1/8 (12.5%) carpi at 6 weeks and 2/12 (17%) at 10 weeks. Histomorphometry showed bridging and reconnection of 5/8 (62.5%) ligaments at 6 weeks and 7/8 (87.5%) ligaments at 10 weeks.
Related Product:
R3ACT™ Stabilization System
Union rates with the use of structural allograft in Lapidus arthrodesis: a comparison between two fixation constructs
Heifner JJ, Rodriguez Materon S, Zhang L, San Giovanni TP,
The Journal of Foot and Ankle Surgery, 2022
A retrospective review was conducted on 91 feet (80 patients) who underwent 1st TMT arthrodesis with and without a PRESERVE™ Lapidus Angular Length Restoring Graft in conjunction with a medial locking plate (Gorilla® Lapidus Plates) or screw fixation. Union was assessed via CT at an average of 15.5 weeks post-op. Union rates were not significantly different between patients who received a PRESERVE™ graft compared to those who did not (90% vs 97%, p=0.41). Union rates were significantly higher for the medial plate group compared to the screw fixation group (98% vs 85%, p=0.04).
Related Products:
PRESERVE™ Bone and Biologic Solutions
Gorilla® Lapidus Arthrodesis System
Dependence of Total Ankle Tibial Baseplate Stability Upon Bone Density
Clarke GA, Johnson JE, de Cesar Netto C, Anderson DD
American Orthopaedic Foot & Ankle Society Annual Meeting, 2023
Finite element analysis (FEA) was used to evaluate micromotions of the tibial component of the APEX 3D(TM) Total Ankle Replacement System. The findings suggest that patient-specific differences in bone density impact implant behavior. Differences due to bone quality were diminished when interference fit was modeled. Interference press-fit has dominant effect on implant stability.
Related Product:
APEX 3D™ Total Ankle Replacement System
Influence of Tibial Component
Design Features and Interference
Fit on Implant-Bone Micromotion
in Total Ankle Replacement: A
Finite Element Study
Influence of sidewall retention and interference fit in total ankle replacement on implant‐bone micromotion: A finite element study
Johnson JE, Clarke GA, de Cesar Netto C, Anderson DD
Journal of Orthopaedic Research, 2024;1-9
Finite element analysis (FEA) was used to investigate factors influencing implant‐bone micromotion in TAR. Differences between implant designs largely disappeared when tibia sidewalls and interference fit were introduced. The results offer novel insight into the effect of TAR fixation features and the associated micromotion at the implant‐bone interface in two patients with representative bone density in their distal tibia.
Related Product:
APEX 3D™ Total Ankle Replacement System
Midterm outcomes of the modified
Lapidus arthrodesis using the
Phantom® Intramedullary Nail
System for the treatment of hallux
valgus
Valdivia JC, Villegas DR
Foot and Ankle Surgery, 2024; 576-581
Fifty-two modified Lapidus procedures performed with the Phantom® Intramedullary Nail were retrospectively reviewed. Intermetatarsal angle, hallux valgus angle, and width of the foot were all significantly improved relative to pre-op. Patients demonstrated significant improvement in AOFAS score, EFAS score, and VAS pain relative to pre-op. One patient experienced a nonunion. There were no reoperations, recurrences, or implant-related complications through the last follow-up.
Related Product:
Phantom® Intramedullary Nail
Overhang, Underhang, and Everything In Between:
Patient-Specific TAR Plans
Paul Cammack, MD; Jeffrey Christensen, DPM; Mathew Anderle, MPH; Laura Brinker, DPM; Donald Hume, PhD
Twin Cities Orthopedics; Integrative Foot & Ankle Centers of Washington; Paragon 28, Inc.
Related Product:
APEX 3D™ Total Ankle Replacement System
Review of Calcaneal Osteotomies Fixed With a Calcaneal Slide Plate
Haggerty EK, Chen S, Thordarson DB.
Foot & Ankle International. 2020;41(2):183-186.
A retrospective review of 81 consecutive patients who underwent either a medial or lateral calcaneal slide osteotomy with a Gorilla® Calc Slide Plate by a single surgeon was conducted. All patients achieved union with no cases of symptomatic hardware. 1 of 81 patients (1.2%) underwent hardware removal after union due to wound breakdown.
Related Product: Gorilla® Calc Slide Plate
Syndesmotic Fixation Utilizing a Novel Screw A Retrospective Case Series Reporting Early Clinical and Radiographic Outcomes
Stenquist D, Velasco BT, Cronin PK, Briceño J, Miller CP, Riedel MD, Kwon JY
Foot & Ankle Specialist. 2020; 13(5), 397-403.
A retrospective review of 18 consecutive patients (with 24 screws) who underwent syndesmotic fixation utilizing a Paragon 28® R3LEASE™ screw was conducted. Mean follow-up was 11.7 months (range: 6.0-14.7 months). 5 of 24 R3LEASE™ screws were broken at an average of 154.8 days (range: 80-196 days) after implantation. All 5 R3LEASE™ screws broke at the intended break point. There was no syndesmotic diastasis, mortise malalignment, or surgical complications. No R3LEASE™ screws were removed.
Related Product: R3LEASE™ Stabilization System
Complications and Early-Term Radiographic Analysis of a Novel Active Compression Tibiotalocalcaneal Arthrodesis Nail With a Proximal Flexible Coil
Anastasio AT, Wu KA, Luo EJ, de Cesar Netto C, Easley ME
Foot & Ankle Orthopaedics, 2025; Vol. 10(1) 1-9
Twenty-one patients who were implanted with a Phantom ActivCore Nail were retrospectively reviewed. Structural allograft was used in 76.2% of cases, and a metal cage was used in 9.5%. 42.8% of the cases were revision procedures. Union rate was found to be 90.4%. Two patients required a secondary surgical intervention. The inner core of the nail experienced 2.5 mm of displacement at 3 months post-op, on average.
Related Product: Phantom® ActivCore™ Nail